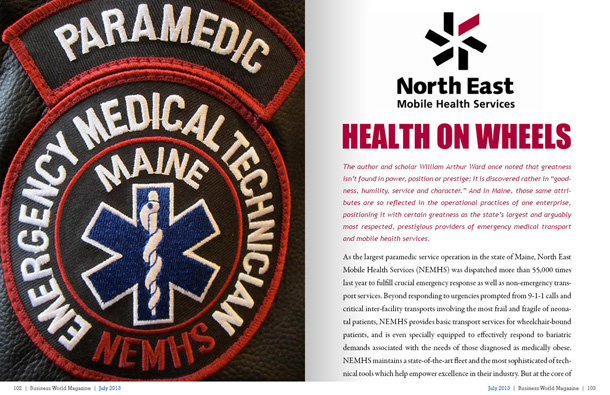
Health on Wheels
The author and scholar William Arthur Ward once noted that greatness isn’t found in power, position or prestige; it is discovered rather in “goodness, humility, service and character.†And in Maine, those same attributes are so reflected in the operational practices of one enterprise, positioning it with certain greatness as the state’s largest and arguably most respected, prestigious providers of emergency medical transport and mobile health services.
As the largest paramedic service operation in the state of Maine, North East Mobile Health Services (NEMHS) was dispatched more than 55,000 times last year to fulfill crucial emergency response as well as non-emergency transport services. Beyond responding to urgencies prompted from 9-1-1 calls and critical inter-facility transports involving the most frail and fragile of neonatal patients, NEMHS provides basic transport services for wheelchair-bound patients, and is even specially equipped to effectively respond to bariatric demands associated with the needs of those diagnosed as medically obese. NEMHS maintains a state-of-the-art fleet and the most sophisticated of technical tools which help empower excellence in their industry. But at the core of North East is a team of people who not only embody the industry’s fullest measure of professional paramedic training, but also the exceptional, if not extraordinary, commitment to respond to the call of duty with both compassion and expert capability. NEMHS is also a dynamic trendsetter and some of the programs it advances have potential to become national service models in the era emerging from adoption of the Patient Protection and Affordable Care Act. The evolution of this enterprise and its expanding role in influencing the global evolution of health services is a story that essentially begins with a winter camping excursion that took place a little more than thirty years ago.
The Emergence of NEMHS
In 1982, Charlie McCarthy was a teenager who had just earned a scholarship to participate in the winter program of Outward Bound. The experience was so enriching that McCarthy imagined himself becoming an Outward Bound Instructor, a position which necessitated emergency medical technician training. After completing initial courses, McCarthy learned that a local volunteer ambulance service was in need of EMTs. He signed up, was assigned to a crew and fell so thoroughly in love with the job that he soon forgot all about Outward Bound. He went on to complete additional training to become a nationally registered paramedic, and later enrolled in Health Service Management courses at the University of Maryland; in fact, he earned his degree during the very same year that he founded Capital Ambulance, serving the Maine communities of Augusta and Bangor. Capital Ambulance was not only the first service in Maine to implement a Critical Care Transport program, but was also the first to create a neonatal transport program, in collaboration with Eastern Maine Medical Center. In 1995, Capital Ambulance secured acclaim as a recipient of the Governor’s Business Excellence Award.
Throughout all that time, Dennis Brockway was directing operations at Delta Ambulance, one of Maine’s largest not-for-profit services. Much like McCarthy, Brockway was smitten by the profession when he was a teenager. In 1971, Brockway was only 16 years old (and only trained in Red Cross First Aid) when he began working for Arrow Ambulance of Waterville. Being called to action, and reveling in that awareness that comes from helping others and knowing your role in alleviating their pain; proved so enticing to Brockway that it also inspired him to become an EMT. He was only 17 when he began working at Delta Ambulance, serving 15 years as a field paramedic and supervisor before becoming its Executive Director. Brockway not only helped expand Delta’s service area from Waterville into the communities of Augusta and Farmington, but was also instrumental in creating the Maine Ambulance Association (MAA) where he currently holds the position of Vice President. Today, he is also a member of the American Ambulance Association and presides on its Regulatory and Legislative Subcommittee, not to mention serving on a variety of other boards affiliated with health services, but again, that’s today. Almost 20 years ago, Brockway sensed that the future would compel alternative approaches to the delivery of EMS services and he found someone of like mind, spirit and expertise in Charlie McCarthy. These two banded together to create North East Mobile Health Services.
Over the same years that Brockway and McCarthy were honing their skills, and long before NEMHS responded to its first dispatch, there was another visionary individual who had been amassing valuable experience and industry distinction as a licensed EMT and paramedic serving communities from Rhode Island and New York to Maine. Kevin McGinnis had been an ambulance service chief for volunteer and hospital-based initiatives, a regional EMS coordinator and a hospital emergency department director before his appointment as EMS Director for the state of Maine, a position he held from 1986 to 1996. McGinnis had hands-on experience in the developing of EMS systems two other states, skills that would ultimately prove essential as NEMHS sought to create a new medical helicopter service. McGinnis joined with Brockway and McCarthy, and over the next few years this team guided NEMHS through the advancing of initiatives that have since taken on lives of their own. The medical air service was established, and ultimately evolved into a separate non-profit, known as LifeFlight of Maine. This was accomplished in concert with another North East colleague, Thomas Judge, who went on to become LifeFlight’s nationally renowned director.
They also devised an entirely new approach to the dispatching of medical care by creating a full service medical emergency communication center known as MEDCOMM. Instead of simply engaging traditional phone operators, MedComm’s team of triage nurses could respond to the myriad health concerns posed by callers. McGinnis says that service ultimately proved to be a little ahead of its time. The nursing side of the operation was eventually separated and transitioned to another enterprise established in Portland, Maine, yet MedComm still continues as a vital communication center for five separate ambulance companies, as well as the medical helicopter service, in Maine.
Community Capability
NEMHS continued to grow as a paramedic service after McGinnis departed from NEMHS, but his reputation in the industry also continued to grow. He would go on to serve as a communications technology advisor for such esteemed organizations as the National Association of State EMS Officials, the National EMS Management Association, the National Association of EMTs, the National Association of EMS Physicians, and the National Association of EMS Educators. Most recently, McGinnis has even been named to the Board of Directors of the First Responder Network Authority (FirstNet), which is presently engaged in building a nationwide public safety broadband network (that is projected to become the largest such system after Verizon, AT&T, Sprint and T-Mobile). He has also served on several public safety bodies of the Federal Communications Commission, including the Joint Advisory Committee on Communications Capabilities of Emergency Medical and Public Health Care Facilities and the Communications Security, Reliability & Interoperability Council. A past Chairman of the U.S. Department of Homeland Security’s SafeCom Program, McGinnis serves on the governing board of the National Public Safety Telecommunications Council. He is also a widely published authority and national speaker on topics involving public safety/EMS communications, rural EMS, and air-medical systems. McGinnis is also recognized as a leading authority on a medical services trend known as “Community Paramedicine,†in fact, he is credited with coining this term, which expands on concepts McGinnis covered in authoring the groundbreaking book Rural/Frontier EMS Agenda for the Future.
In expounding on community paramedicine, McGinnis explains that when reviewing the totality of incoming 9-1-1 calls, as many as 40 percent may involve something other than a medical emergency. McGinnis refers to these situations as “unscheduled medical service†which can be prompted from someone who is simply ill, or who has experienced a non-injury fall, or requires some type of service which is not necessarily a medical emergency. In such cases, it may not actually be necessary, nor even advisable, to transport the person to a hospital emergency room; the caller may simply require services which can be addressed by a community paramedic professional who might ultimately refer the person to services rendered by other agencies. In some cases, a person may not be acutely sick today, but if medical treatment isn’t provided, the person will be sick tomorrow, thus generating a call to 9-1-1. Community paramedicine not only strives to provide a means of care delivery that helps prevent emergency dispatch of services, but also serves to connect patients with services more aligned with their immediate needs. Community paramedics also undergo training, and can be dispatched to scenes alongside EMS paramedics, but after assessing the situation can provide services which would be more appropriate than sending a person to emergency rooms which may be sufficiently busy tending to more urgent needs. Community paramedicine programs have been adopted in areas such as Pittsburgh, Fort Worth and Wake County, North Carolina, and McGinnis anticipates that trend to increasingly sweep throughout the country.
McGinnis returned to NEMHS (as Chief) two years ago to help the company transition from an emergency and non-emergency transport service, into a full-fledged mobile health service. Since his return, NEMHS has become the first ambulance service to secure approval of a pilot project involving community paramedicine as a means to decrease the risk of injury from falls. As McGinnis explains, in some cases, a senior may fall, but not incur injuries that result in a trip to the emergency room, in fact, he or she may refuse hospital care altogether. The person may be fine for now, but the next fall could lead to a broken hip or some other injury which prompts all manner of other medical services. So, in the appropriate situation, the community paramedicine provider would meet with the patient to determine the nature of the fall, assessing whether it was caused by some issue involving mobility, stability, a vision problem, reaction to prescription, or environmental factors such as a loose rug or other impediment. The provider will meet with the person in his or her home to make recommendations and the information is also shared with the person’s personal physician so that he or she can also make any necessary recommendations. The intent is to help spare the person from falling again. That not only benefits the individual who could suffer from a fall, but reduces the demand on emergency medical services and hospital resources. McGinnis says the idea has resonated not only with medical professionals, but insurance companies too.
NEMHS is also beginning another community paramedicine project which poses benefits for people recovering from severe injuries requiring surgical intervention. McGinnis explains that following “trauma†surgery at the Maine Medical Center (a Maine EMS designated trauma center), a person may be discharged from the hospital and have a long trip to return home. This is because patients often come by ambulance and helicopter to the trauma center from long distances for the specialty care they desperately need. After discharge, the person may be required to routinely check in with a doctor over the following weeks, necessitating a repeat of that long drive to the trauma center clinic simply to have an examination that lasts for only a few minutes. In this new program, the community paramedic trained in postsurgical evaluation could meet with such individuals within their own homes, assess their injuries and recovery, and spare them from the trip to the doctor. Equipped with an iPad and video link, the community paramedic could help facilitate the exchange that would allow the surgical nurse practitioner to monitor the patient’s recovery via video link. It’s fast and convenient.
McGinnis says these and other community paramedicine programs continue to spread throughout the country. He anticipates that changes in healthcare, coupled with reductions in budgets and diminishing reimbursement rates from agencies such as Medicaid and Medicare will prompt new innovations and new efficiencies in the delivery of healthcare services. The business model, particularly billing, has yet to be worked out with respect to community paramedicine. McGinnis suspects that it will rely on a fee-for-service model early on, but he notes that in Minnesota, Medicaid has allowed for reimbursements to community paramedicine providers. Medicare has also begun funding several grants involving the concept. McGinnis says in the future, where hospitals and insurance companies will realize cost savings through the interventions provided by community paramedicine providers, they may choose to direct a portion of those savings to cover the cost of the care that was provided, but that’s the future, and it’s a future that is not that far away. McGinnis concedes that these concepts may seem scary to those clinging to the methodologies of old. “This is threatening to those living in the world of yesterday,†he says. “In the world of tomorrow, traditional revenue streams no longer hold, whether that’s in the form of government funding or a fee for service which relies on reimbursements from third party payers. From what I see, municipal governments are increasingly challenged finacially. I don’t see them increasing public service funding..†To that point, Medicare has cut ambulance reimbursements by two percent this year because of sequestration. They will also soon cut reimbursement relating to ambulance transports involving dialysis treatment by ten percent. As McGinnis says, “We’re looking at decreases. Conventional revenue streams are no longer dependable. Community paramedicine poses a means to not only create a more dependable revenue stream consistent with the healthcare system of tomorrow, but also a means of delivering great patient care, while also improving the level of healthcare for an entire population, enhancing patient satisfaction, lowering costs and effecting saving in the continuum of healthcare services.â€
McGinnis is today among the first class of students who will become Maine’s first Community Paramedics. NEMHS has becoming a leading provider of training affiliated with this increasing trend, as well as a variety of other health and safety classes branded through a program that promotes the ability for participants to go “From Zero to Hero.â€
Excellence in their Industry
Beyond the extensive training, consulting and industry advising, NEMHS is a full service provider compelled by the whole package in terms of critical services it provides. They’ve invested heavily in the resources of licensed personnel, equipment and technological resources to effectively respond to emergency transport needs. Those functions are furthered by specialized teams uniquely trained to respond to the direst of medical urgencies, the transport needs of bariatric patients, as well as neonatal patients served by the NEMHS “Angel Teamâ€, a partnership with the Barbara Bush Children’s Hoapital at Maine Medical Center. A new North East neonatal vehicle, put into service this month, can accommodate two isolettes allowing for double occupancy, and is one of the biggest such units in the nation. The Service also sponsors “North East Mountain Rescue†a high-angle rescue team that provides access to patients trapped on cliffs and other dangerous settings. It also has a specialized team that can respond several staffed ambulances to mass casualty incidents in Maine and elsewhere (they were activated, but not used, in the Hurricane Sandy response in New Jersey).
On the technology side, NEMHS relies on the industry’s greatest offerings in tools to rapidly get a GPS fix on dispatch locations, and deploys triple-redundancy in the receiving of emergency calls, allowing a dispatch indication to not only come in by way of their radio handsets, but also their smart phones and in-vehicle computers known as NOMAD. The device, the industry-specific software that drives it, as well as the cardiac monitor systems are among the technical innovations NEMHS has acquired through its relationship with Zoll Medical Corporation, a leading supplier of medical devices and software solutions. NEMHS is also strengthened by solutions secured from Active Communications, Inc., a provider of public safety radio communications, systems network-design services and, as wide-area digital commercial “two-way†communication devices. Through a contract with another company known as BizCompass, NEMHS is complemented with services from a Chief Technology Officer who participates in all staff meeting (as if he were a full time employee) but essentially serves to provide oversight of the sophisticated IT systems. McGinnis says the arrangement allows for a lot of technological capability, but without a lot of the costs typically associated with such infrastructure and expert support.
While NEMHS is dedicated to providing crucial support to the patients that rely on its services, McGinnis notes that his team is also mindful of the sacrifices which are made daily by everyone who works in his service field. Some eight years ago, McGinnis says his team realized that while statewide memorials had been erected to honor police and fire personnel who had died in the line of duty, there was no such memorial for EMS staff. Tragically, each year, there are EMS personnel who die due to accidents in air or over-the-road operations. There are also professionals whose contributions in EMS, whether as a doctor, nurse, paramedic or heath systems developers, have made an incredible and indelible impact on countless lives. McGinnis approached the Maine Legislature to garner approval to create a new memorial honoring the Maine EMS system, its founders and those who make it succeed every day. Located along the police and fire memorials on the state capitol grounds, this one is not the typical granite stone edifice, but consists of a clear glass Star of Life panel, the international symbol of emergency medical services. This star will be lit at night, and the site is complemented by granite and glass columns that will also be lit. Smart phone applications allow visitors to connect with an audio tour and listen to EMS providers, nurses or doctors, who will share their perspective on their professional roles. The audio component for those who have fallen in the line of duty features colleagues and family memories of the fallen professional. As McGinnis says, “There’s no other memorial quite like this one.â€
And that’s fitting, because the people who work in emergency medical services are like none other. McGinnis observes, “You don’t normally hear too much or see what paramedics do. They’re inside a hospital or at a base, and most people don’t think about them until 9-1-1 is called, but then they’re always there when you need them and they do what needs to be done. They’re very special people and their work saves and improves lives.â€
For more information, please visit their website at: Â North East Mobile Health Services
Preferred Vendors of Choice: